The Link Between Endometriosis and Migraine
Posted on March 05 2024,
A new study published in the journal Cephalalgia took a closer look at the relationship between endometriosis, adenomyosis (endometriosis within the uterine muscle), and migraine in premenopausal women not taking hormonal treatments.
Using ultrasound imaging and neurological exams, the researchers found that women with both endometriosis/adenomyosis and migraine experienced far more severe symptoms and disability compared to those with just one of the conditions alone. This included higher pain levels, more frequent migraine episodes, and significantly greater impact on daily activities.
The researchers also observed a much higher prevalence of severe adenomyosis and deep infiltrating endometriosis lesions in the abdomen and pelvis among the women with both endometriosis and migraine. These more invasive endometriosis types seemed to be fueling the heightened migraine severity and comorbidity burden.
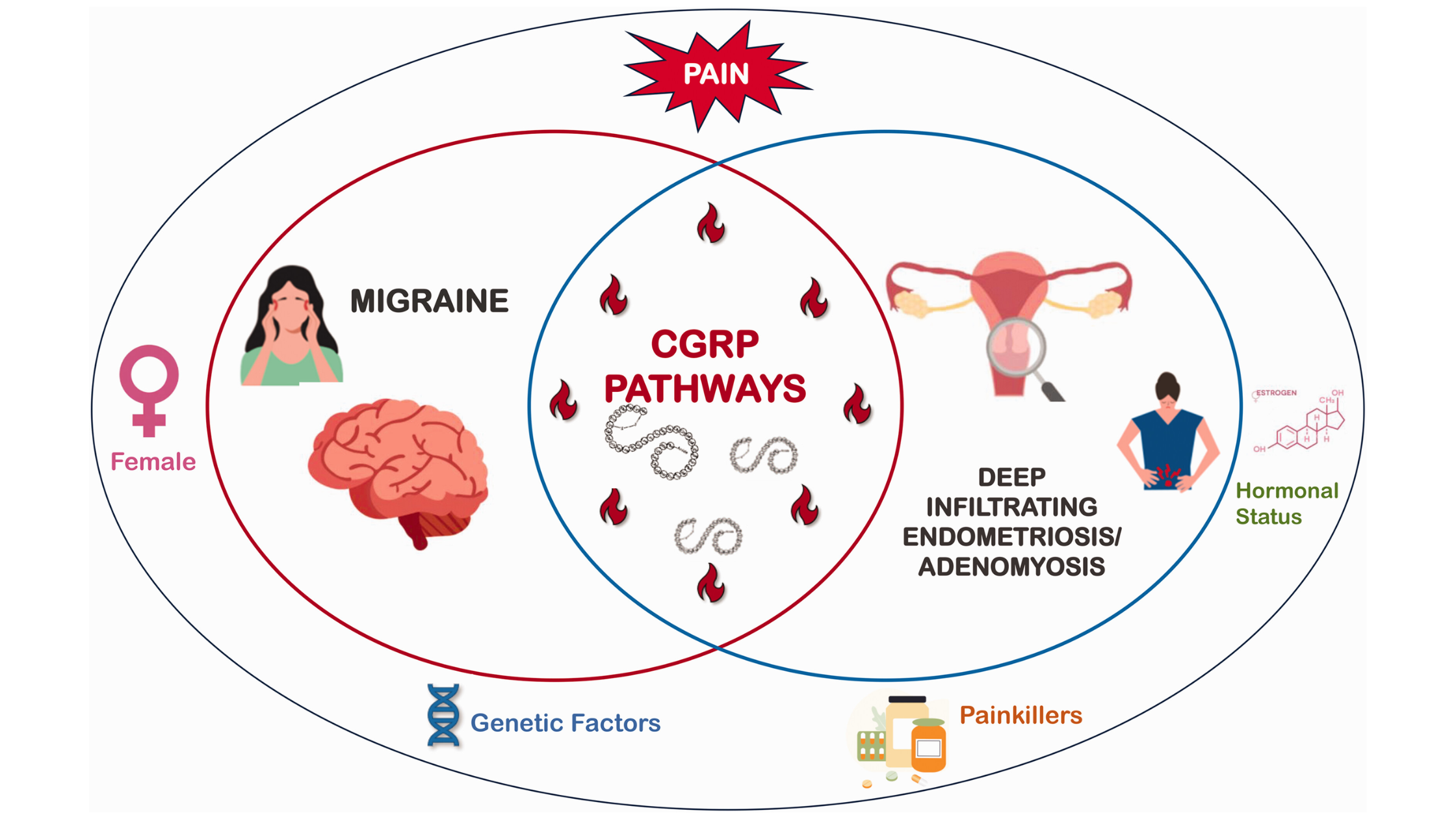
So, what could explain this link? The study authors point to possible shared inflammatory pathways involving calcitonin gene-related peptide (CGRP), a key neurotransmitter implicated in both endometriosis pain and migraine attacks. Essentially, the deep endometriosis lesions may promote a perpetual state of neurogenic inflammation that feeds into more severe and frequent migraine episodes.
An equally concerning finding was that migraine often preceded the diagnosis of endometriosis by years in this patient group, suggesting both conditions were going unrecognized and untreated for a long time. The researchers emphasize the need for earlier multidisciplinary screening and workup when either migraine or endometriosis symptoms first appear in young females.
By taking a comprehensive approach, combining ultrasound evaluation for endometriosis along with migraine assessment, these disabling comorbidities could be caught sooner. This would then open the door for more timely treatment - whether that involves hormonal therapies, anti-inflammatory medications, CGRP inhibitors, or other approaches tailored to each the patient’s specific condition and needs.
This study suggests that endometriosis and migraine should no longer be viewed as separate issues for females experiencing both. There are likely similar pathophysiological and biological connections influencing their co-existence and severity. Increasing awareness of this important link will hopefully lead to better multidisciplinary care and improved quality of life for the many females with impacted by this dual burden of chronic pain.
Wed, Jan 14, 26
New Emergency Department Migraine Treatment Guidelines
The American Headache Society (AHS) has released its 2025 guideline update for the acute treatment of migraine in adults presenting to the emergency department. This update, published in Headache in...
Read MoreSun, Jan 04, 26
Long-Term Safety of Anti-CGRP Monoclonal Antibodies
A comprehensive meta-analysis of over 4,300 patients reveals that erenumab, galcanezumab, fremanezumab, and eptinezumab maintain good tolerability beyond 12 months. Only 3% of patients stopped treatment due to adverse events,...
Read MoreThu, Jan 01, 26
Alternate Nostril Breathing Protocol for Migraine
Alternate nostril breathing is a simple yogic technique that's showing real promise for migraine prevention. Unlike acute treatments, this practice builds nervous system resilience over time - making attacks less...
Read More


