Understanding the Link Between Endometriosis and Migraine
Posted on April 18 2025,
Understanding the Link Between Endometriosis and Migraine
New systematic review and meta-analysis reveals a significant connection between these two conditions and what it means for patients
The Research Overview
A new systematic review and meta-analysis has found a significant link between endometriosis and migraine headaches. The researchers analyzed data from 13 different studies involving 331,655 individuals (32,489 with endometriosis and 299,166 controls) to examine this relationship.
This comprehensive study sought to quantify the risk of migraine in those with endometriosis, while also investigating how factors like endometriosis severity, location, and migraine subtypes affect this association.
Why This Matters
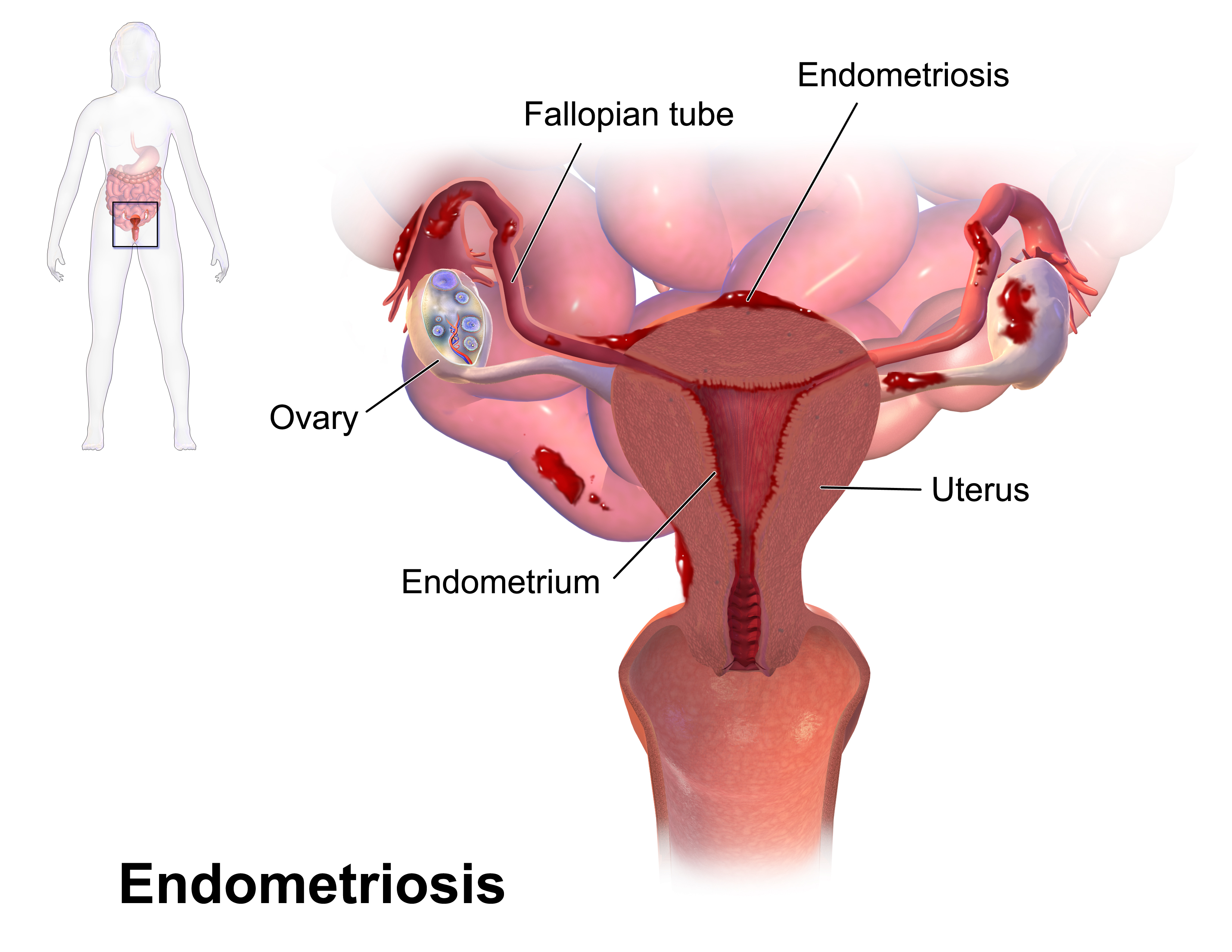
Endometriosis affects approximately 10% of women of reproductive age, while migraine affects 20% of women. Understanding the connection between these conditions could improve diagnosis and treatment for millions of people worldwide.
Key Findings
The research revealed several important discoveries about the relationship between endometriosis and migraine:
The study also found that different types of endometriosis had varying levels of association with migraine. This suggests that certain forms of the condition may share stronger biological links with migraine headaches.
Endometriosis Location & Severity
The location and severity of endometriosis appears to significantly impact the likelihood of experiencing migraine headaches:
Data from Maitrot et al., 2020 study included in the meta-analysis
Data from Wu et al., 2022 study included in the meta-analysis
These findings suggest that more severe forms of endometriosis and those affecting specific locations in the body have a stronger association with migraine. This may help doctors identify patients at higher risk.
What This Means for Patients
These findings have important implications for both people with migraine and those with endometriosis:
If You Have Migraine
Be aware of endometriosis symptoms: If you experience pelvic pain, painful periods, pain during intercourse, or infertility, discuss these symptoms with your healthcare provider. They may be signs of endometriosis, which occurs at higher rates in migraine patients.
Consider specialized gynecology care: Women with migraine, particularly migraine without aura, should discuss possible endometriosis screening with their doctors, especially if they have any pelvic pain symptoms.
Track your menstrual cycle: If your migraine disease worsens around your period, this could signal hormonal involvement that may also be connected to potential endometriosis. Tracking can help identify patterns for both conditions.
If You Have Endometriosis
Be aware of migraine symptoms: If you experience recurrent headaches, especially with nausea, sensitivity to light or sound, or visual disturbances, discuss these symptoms with your healthcare provider. They may represent migraine, which occurs at more than twice the rate in endometriosis patients.
Know your risk: Understanding that more severe forms of endometriosis are associated with a higher migraine risk (up to 4.5 times higher) can help you be more proactive about discussing headache symptoms with your healthcare team.
Share your endometriosis diagnosis: When seeing healthcare providers for headaches, make sure they know about your endometriosis diagnosis, as this may influence their assessment and treatment approach.
For All Patients
Consider coordinated care: The strong association between these conditions suggests possible shared biological mechanisms. A treatment approach that addresses both conditions may be beneficial.
Advocate for comprehensive evaluation: When one condition is diagnosed, ask about screening for the other, particularly if you have any suspicious symptoms.
Watch for hormonal patterns: Both conditions can be influenced by hormonal fluctuations. Tracking your symptoms in relation to your menstrual cycle may help identify patterns and guide treatment decisions.
While this research shows a clear association between endometriosis and migraine, not everyone with one condition will develop the other. However, being aware of this connection can help you seek appropriate care if symptoms arise.
Potential Shared Mechanisms
The study authors suggest several potential biological mechanisms that might explain the connection between endometriosis and migraine:
Estrogen plays a crucial role in endometriosis by promoting the growth of endometrial tissue. Similarly, estrogen fluctuations have been suggested to trigger migraine attacks. Both conditions are influenced by hormonal fluctuations during the menstrual cycle.
Achieving amenorrhea (absence of menstruation) through hormonal treatments has been shown to reduce menstrual-related migraine attacks. This suggests that hormonal management strategies might benefit both conditions simultaneously.
Endometriosis triggers an inflammatory response with elevated levels of prostaglandins, cytokines, and chemokines. This inflammatory environment operates not only within the peritoneal cavity but also at a systemic level.
Migraine similarly involves inflammation, with local inflammation triggering meningeal nociceptors and activating the trigeminovascular system. Both conditions show elevated levels of inflammatory markers, suggesting inflammation may be a common pathway.
Growing evidence indicates a genetic link between endometriosis and migraine. Genome-wide association studies have identified multiple genetic markers associated with both conditions.
A study in twins found a significant genetic correlation between endometriosis and migraine, suggesting shared genetically controlled biological mechanisms that may predispose individuals to both conditions.
Reference: Colombo GE, Makieva S, Somigliana E, et al. The association between endometriosis and migraine: a systematic review and meta-analysis of observational studies. The Journal of Headache and Pain. 2025;26:82. https://thejournalofheadacheandpain.biomedcentral.com
Mon, Nov 17, 25
Migraine Research - During the week of my absence.
Migraine Research - During the week of my absence. The Association Between Insomnia and Migraine Disability and Quality of Life This study examined how insomnia severity relates to migraine disability...
Read MoreSat, Nov 01, 25
Anti-CGRP Monoclonal Antibody Migraine Treatment: Super-Responders and Absolute Responders and When to Expect Results
Anti-CGRP monoclonal antibodies achieved 70% super-response and 23% complete migraine freedom in a one-year study. Most dramatic improvements occurred after 6 months of treatment. For patients with chronic or high-frequency...
Read MoreAll Non-Invasive Neuromodulation Devices for Migraine Treatment
Wondering if migraine devices actually work? This guide breaks down the latest evidence on non-invasive neuromodulation devices like Cefaly, Nerivio, and gammaCore. Learn which devices have solid research backing them,...
Read More



