Migraine Attacks Independent of CGRP (cGMP-mediated migraine)
Posted on June 09 2024,
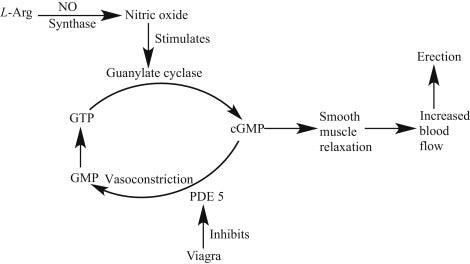
A randomized, double-blind, placebo-controlled study published in Cephalalgia investigated whether sildenafil (Viagra), a phosphodiesterase-5 (PDE-5) inhibitor that increases cGMP levels, could induce migraine attacks in individuals with migraine who were pre-treated with erenumab (Aimovig), a calcitonin gene-related peptide (CGRP) receptor monoclonal antibody.
The study found that 63% of participants experienced a migraine attack within 12 hours after taking sildenafil, compared to only 19% after taking placebo. These findings suggest that the cGMP pathway can trigger migraine attacks INDEPENDENTLY of CGRP receptor activation.
The clinical implications of this study are significant. First, it emphasizes that migraine pathophysiology is complex and involves multiple signaling pathways. Second, it highlights the cGMP pathway as a potential target for future migraine treatments, particularly for patients who do not respond adequately to CGRP-targeted therapies or experience side effects from these treatments.
The study also raises the possibility of developing personalized migraine treatments based on an individual's predominant migraine-triggering pathways. Patients with migraine primarily driven by the cGMP pathway might benefit more from therapies targeting this pathway, while those with CGRP-driven migraine might respond better to CGRP-targeted treatments. Furthermore, combination therapies targeting both pathways simultaneously might provide increased efficacy for some patients (this is currently being studied with anti-PACAP and anti-CGRP drugs).
While the specific mechanisms by which cGMP contributes to migraine pathogenesis remain to be fully known it may be easy to jump to the conclusion that it is vasodilation due to the mechanism of action and clinical outcome of sildenafil. However, the study's authors discuss potential sites of action of sildenafil within the trigeminovascular system. They note that sildenafil, being a lipophilic drug, can cross the blood-brain barrier and exert central effects, potentially activating excitatory neuronal pathways that may contribute to migraine attack initiation. Remember, migraine is neurovascular, not solely vascular in pathogenesis.
It is important to note that this study is small and further research is needed to confirm these findings and fully understand the clinical implications of targeting the cGMP pathway in migraine management.
Wed, Jan 14, 26
New Emergency Department Migraine Treatment Guidelines
The American Headache Society (AHS) has released its 2025 guideline update for the acute treatment of migraine in adults presenting to the emergency department. This update, published in Headache in...
Read MoreSun, Jan 04, 26
Long-Term Safety of Anti-CGRP Monoclonal Antibodies
A comprehensive meta-analysis of over 4,300 patients reveals that erenumab, galcanezumab, fremanezumab, and eptinezumab maintain good tolerability beyond 12 months. Only 3% of patients stopped treatment due to adverse events,...
Read MoreThu, Jan 01, 26
Alternate Nostril Breathing Protocol for Migraine
Alternate nostril breathing is a simple yogic technique that's showing real promise for migraine prevention. Unlike acute treatments, this practice builds nervous system resilience over time - making attacks less...
Read More


