Groundbreaking study!: Anti-CGRP Monoclonal Antibodies Disease-Modifying!?
Posted on January 26 2025,
I-GRAINE Study: Anti-CGRP Antibodies Show Disease-Modifying Properties
The recent I-GRAINE study provides evidence that anti-CGRP monoclonal antibodies may have disease-modifying properties (that is, it can do more than just manage symptoms) in migraine when used long-term, challenging previous understandings of these treatments.
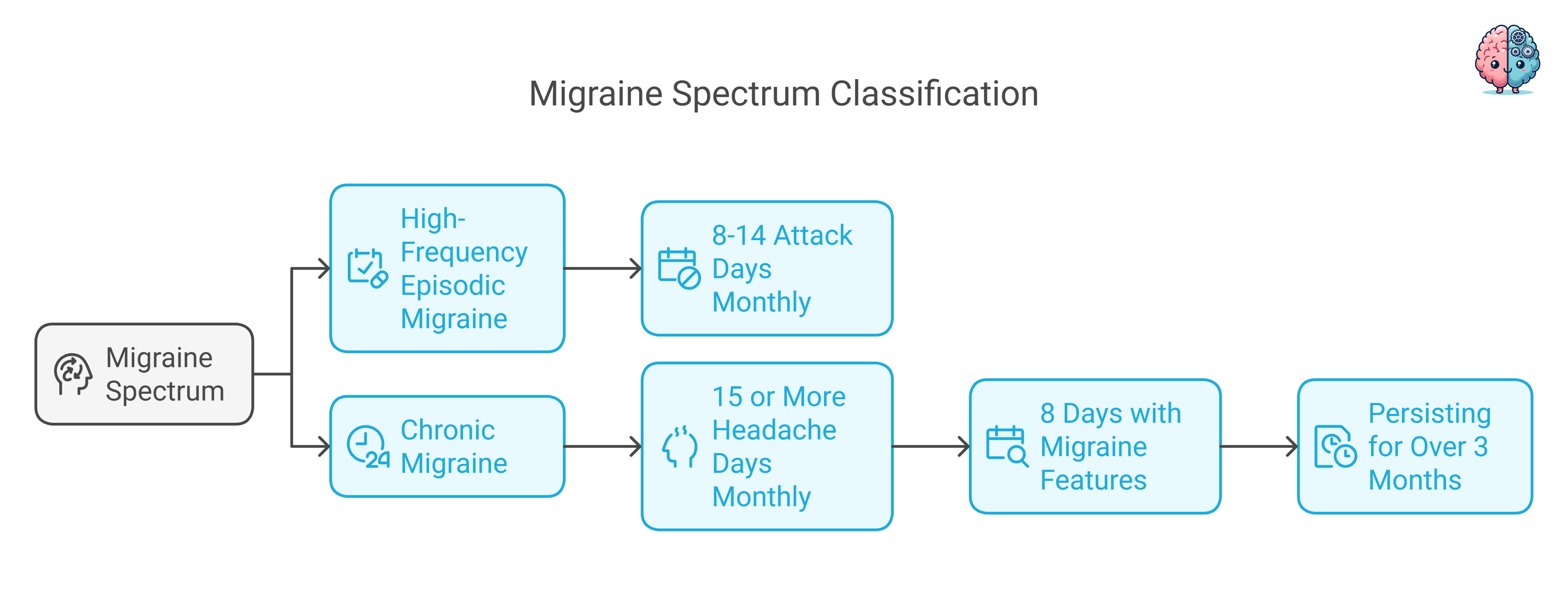
To appreciate the significance of this finding, it's important to understand that migraine exists on a spectrum. High-frequency episodic migraine (HFEM) affects patients with 8-14 migraine attack days monthly, while chronic migraine (CM) has 15 or more headache days monthly, with at least 8 days a month having features of migraine attacks, persisting for over 3 months.
Key Study Parameters

Understanding the Treatment and Study Design
The study followed 212 patients with either HFEM or CM through three years of treatment with anti-CGRP monoclonal antibodies. These medications work by targeting either the calcitonin gene-related peptide (CGRP) itself or its receptor. CGRP is a protein that plays a crucial role in pain transmission and inflammation during migraine attacks. The medications studied included erenumab (Aimovig, which blocks the CGRP receptor) and galcanezumab (Emgality) or fremanezumab (Ajovy, both of which block CGRP itself), all administered as monthly subcutaneous injections.
Remarkable Progress in Migraine Management
What makes the findings especially exciting is the progressive improvement in treatment response across discontinuation periods after each yearly treatment cycle (discontinuation of anti-CGRP mAbs is not recommended and needs to be addressed. However, in Italy, and most of Europe, discontinuation is standard practice). The percentage of patients maintaining a 50% or greater reduction in migraine days during the first month after treatment discontinuation increased dramatically from 25% after the first year (D1), to 53.8% after the second year (D2), and reached 77.8% after the third year (D3).
Measuring Treatment Success
The researchers measured several key indicators of migraine burden. These included monthly migraine days (MMD), monthly headache days (MHD), monthly analgesic intake (MAI), pain intensity using a numerical rating scale (NRS), and impact on daily life using the Headache Impact Test (HIT-6). All these measures showed improvements over the three-year period.
Breakthrough Results and Implications
The reduction in relapse rates to chronic migraine is one of the most significant aspects of this study - from 67.7% after the first year to just 2.3% after the third year. Similarly, medication overuse/adaptation headache, a complication where frequent use of pain medications actually worsens headaches, dropped from 34.2% to 1.3%. These findings strongly suggest that prolonged treatment with anti-CGRP monoclonal antibodies may be altering the underlying disease process.
Dramatic Reductions in Complications
- Chronic migraine relapse: From 67.7% to 2.3% over three years
- Medication overuse headache: From 34.2% to 1.3% over three years
- Treatment response: Progressive improvement from 25% to 77.8%
- Sustained benefits: Effects persisted even after treatment discontinuation

Other Studies Say Otherwise
The proposed mechanism involves a gradual desensitization of pain pathways over time, moving beyond symptom control to potentially modifying the migraine disease course itself. Therefore, this study suggests that these medications induce lasting changes in migraine pathophysiology when used for extended periods.
Important Consideration
However, it's important to note that previous studies disagree with the disease-modifying progress of anti-CGRP mAbs. This apparent contradiction actually helps explain why duration of treatment may be crucial - the disease-modifying effects may only become apparent with longer treatment periods that allow for gradual desensitization of pain pathways and neuroplastic changes. This study suggests that one year may not be long enough to achieve these lasting changes, while three years of treatment may allow for more fundamental modifications to the underlying disease process.

Ultimately, more research, particularly randomized controlled trials with extended follow-up periods, would be needed to definitively prove the disease-modifying properties of these medications and to identify which patients are most likely to benefit from extended treatment periods.
If confirmed by further studies, this could mark a significant shift in how we approach long-term migraine management.
Source: I-GRAINE Study - Journal of Neurology
Read the Full StudyWed, Jan 14, 26
New Emergency Department Migraine Treatment Guidelines
The American Headache Society (AHS) has released its 2025 guideline update for the acute treatment of migraine in adults presenting to the emergency department. This update, published in Headache in...
Read MoreSun, Jan 04, 26
Long-Term Safety of Anti-CGRP Monoclonal Antibodies
A comprehensive meta-analysis of over 4,300 patients reveals that erenumab, galcanezumab, fremanezumab, and eptinezumab maintain good tolerability beyond 12 months. Only 3% of patients stopped treatment due to adverse events,...
Read MoreThu, Jan 01, 26
Alternate Nostril Breathing Protocol for Migraine
Alternate nostril breathing is a simple yogic technique that's showing real promise for migraine prevention. Unlike acute treatments, this practice builds nervous system resilience over time - making attacks less...
Read More


